DO HERBS, VITAMINS, AND ANTIOXIDANTS ADVERSELY AFFECT CANCER THERAPIES?
preliminary report by Subhuti Dharmananda, Ph.D., Director, Institute for Traditional Medicine, Portland, Oregon
For more than 30 years now, Chinese herbs and materials derived from the herbs, such as long chain polysaccharides, have been used as adjunct therapies for cancer patients. This modern application was first developed clinically in China and Japan during the 1970s and was relayed to the rest of the world in 1983 through an international conference in Beijing which was followed up by press reports in English and other languages (see: Physiological responses to immunologically active polysaccharides). The Institute for Traditional Medicine (ITM) made an effort to alert practitioners of Chinese medicine in the U.S. to this promising role for Chinese herbs immediately after that conference, with updated information provided as available over the years. The utilization of Chinese roots, leaves, and fruits (e.g., astragalus, gynostemma, ligustrum, and lycium), and several mushrooms (e.g., coriolus, ganoderma, cordyceps, and lentinus) for cancer patients is now a routine procedure when these patients visit acupuncturists, naturopathic physicians, and others offering adjunctive cancer health care.
Within the past couple of years, however, an increasing number of patients have been told by their oncologists to avoid herbs, and to more generally avoid supplements (such as vitamins), or, even more broadly, simply avoid anything with antioxidant potential while they are undergoing cancer therapies. The admonition itself is difficult to interpret, since all foods contain antioxidants and vitamins, and they also contain most of the other substances offered in dietary supplements. Most fruits, vegetables, beans, and nuts differ only slightly from herbs. A more specific recommendation is needed. But first, the question arises: why are doctors giving these instructions? What kind of information is being released to the public?
I have attempted to trace back the origins of the restrictions imposed by some oncologists, and it seems that the primary instigator of the concern was Dr. David Golde at the Memorial Sloan-Kettering Cancer Center, even though he was not the first to raise the matter (but within a few months of being first). The main issue he raised was the use of high doses of vitamin C, a therapy that has nothing directly to do with herbs. Herbs usually have little or no vitamin C; still, vitamin C is commonly prescribed or recommended as a supplement by practitioners involved in natural healing.
In a June 19, 2000 report of WebMD Medical News, the use of high doses of vitamin C to prevent heart disease, cancer, and other disorders, was called into question, and Dr. Golde's research and comments were relayed (1, 2):
The first of two recent studies that called this notion [of taking high doses of vitamin C as a disease preventive] into question was carried out by David Golde, MD, physician-in-chief at Memorial Sloan-Kettering Cancer Center in New York City, and described at an American Cancer Society meeting in March 2000. Golde and his colleagues transplanted human cancer cells into mice, injected the mice with vitamin C, and then measured the amount of the vitamin in the cells. They found that cancer cells seem to soak up large amounts of vitamin C by converting it into a form that's easier to absorb. The results, Golde says, raise the possibility that cancer cells may use vitamin C to shield themselves against radiation and chemotherapy.
The second study, performed by James Dwyer, Ph.D., an epidemiologist at the University of Southern California, caused an even bigger stir. Dwyer told an American Heart Association meeting in March 2000 that middle-aged men who took 500 milligrams of vitamin C supplements daily showed a rapid narrowing of their carotid arteries, which supply blood to the brain.
The studies sound alarming, but experts warn against making too much of them. While Golde says that cancer patients shouldn't take large doses of the vitamin, other researchers say it's far too early to make that recommendation. There's no evidence yet that C actually shields cancer cells from treatment, says Mark Levine, MD, an endocrinologist and Vitamin C expert at the National Institutes of Health. The cancers tested in Golde's research, he says, may simply have grown from tissues that normally take in large amounts of the vitamin.
As for the heart disease finding, Dwyer himself cautioned that it is preliminary. The study lasted only 18 months and included just 573 men. And Robert Jacob, Ph.D., a research chemist with the U.S. Department of Agriculture, points out that previous studies suggested just the opposite-that vitamin C reduces the narrowing of carotid arteries.
From these very modest beginnings in Spring of 2000, the worry about antioxidants and cancer therapies grew, despite several warnings about the interpretation of data, such as those mentioned in the above analysis, and almost everyone who wished to provide a basis for the antioxidant and vitamin worry seemed to harken back to Dr. Golde's very preliminary research. A pharmacist, John Russo, Jr., wrote the following to caution his readers about the possible interaction of antioxidants with brachytherapy (radiation therapy where the radiation source is placed inside the body) for prostate cancer (3):
How might an antioxidant adversely affect brachytherapy?
The precise role that the antioxidant, vitamin C, plays in tumors is not known, but recent studies have shown possible interactions between dietary antioxidants and cancer treatment.
We know that vitamin C is a powerful antioxidant. It consumes free radicals, the toxic substances in the body that can be generated by chemotherapy agents to destroy cancer cells. "It is possible," according to Dr. David Golde, Physician-in-Chief at Memorial Sloan-Kettering Cancer Center, "that taking large amounts of vitamin C could interfere with the effects of chemotherapy or even radiation therapy." These therapies often kill cells, in part, by using oxidative mechanisms. it's conceivable then, that vitamin C might make cancer treatment less effective, and it is reasonable that cancer patients undergoing chemotherapy avoid taking large amounts of this vitamin."
Building on past research
Earlier research by Dr. Golde and his colleagues established that specific glucose transporter molecules carry vitamin C into cells. This occurs once vitamin C, which is used by cells in the form of ascorbic acid, is converted into dehydroascorbic acid and transported into the cell. Once inside, the vitamin is converted back to ascorbic acid.
Applying this information to patient care
According to David Agus, an oncologist at Memorial Sloan-Kettering Cancer Center, we now know that tumors acquire and retain large amounts of vitamin C. And their nutritional needs appear to be similar to healthy cells that take in large amounts of the vitamin."
However, what cancer cells do with the vitamin C after it is absorbed is not known. This will have to be determined before guidelines for the complementary use of antioxidants during chemotherapy and radiation become established.
Furthermore, research from University of Tubingen, School of Medicine in Germany suggests caution in applying this knowledge to all antioxidants in all types of malignancies. Examination of the modulation of drug-induced cytotoxicity and clonogenic cell death of glioma cells by three structurally unrelated antioxidants revealed that these antioxidants inhibit acute cytotoxicity and clonogenic cell death induced by cisplatin. However, they had little effect on the toxicity of other cancer drugs including BCNU, doxorubicin, vincristine, cytarabine, or camptothecin.
In the discussion of brachytherapy, the pharmacist carries the implications over to chemotherapy agents, but mistakenly states that these function by producing free radicals. In general, this is not the case, and only applies to radiation (see explanation of mechanism, Appendix).
The research cited here about an inhibition of cisplatin therapy by antioxidants (but, notably, no effect of the tested antioxidants on several other chemotherapy drugs) was published in 1998 (4), and did not produce much interest at the time, nor has a follow-up report been published to date (end of 2002). Glioma cells (a type of brain cancer) are normally resistant to the effects of chemotherapy, and the authors were examining factors influencing this already poor response. They determined, in their study, that cisplatin did not rely on free-radical formation to damage glioma cells, so antioxidant activity working directly against cisplatin effects was not an issue. Rather, the substances tested in this in vitro study appeared to function by some other unknown mechanism.
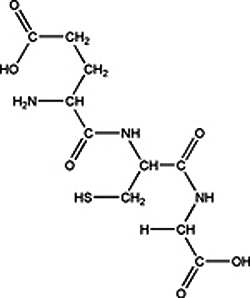
By contrast, another platin drug, oxaliplatin, was used in a double-blind, placebo controlled clinical trial along with administration of the antioxidant glutathione (GSH; see Figure 1). The authors concluded (5): "This study provides evidence that GSH is a promising drug for the prevention of oxaliplatin-induced neuropathy, and that it does not reduce the clinical activity of oxaliplatin."
This is an important finding, because it had been proposed that cancer cells could become resistant to platin drugs (e.g., cisplatin and carboplatin; see Figure 2) due to changes in the cancer cell membrane, where the resistance may be caused by the binding of platinum to intracellular thiols, such as glutathione. This possibility, based on in vitro studies, implies that the interaction between platinum and GSH could prevent the active compounds from reaching the DNA nucleus. It is unclear at this point, whether administering glutathione can be recommended (as is often done by proponents of its protective effects), but this substance does not appear to have any direct interference with oxaliplatin when used clinically based on the recent clinical trial. In vitro studies indicate that high intracellular glutathione levels protect cancer cells from the effects of chemotherapy, but this may not carry over to the clinical situation.
A related concern about chemotherapy drug resistance has been raised about using antioxidants with cyclophosphamide, a particularly toxic anticancer drug. When the literature was reviewed, it was found that, if anything, the substances were beneficial for patients on cyclophosphamide therapy. Here is the interaction caution about this drug as relayed in Healthnotes (6-10):
Interactions with Dietary Supplements
Antioxidants
Cyclophosphamide requires activation by the liver through a process called oxidation. In theory, antioxidant nutrients (vitamin A, vitamin E, beta-carotene and others) might interfere with the activation of cyclophosphamide. There is no published research linking antioxidant vitamins to reduced cyclophosphamide effectiveness in cancer treatment. In a study of mice with vitamin A deficiency, vitamin A supplementation enhanced the anticancer action of cyclophosphamide. Another animal research report indicated that vitamin C may increase the effectiveness of cyclophosphamide without producing new side effects. Preliminary human research found that adding antioxidants (beta-carotene, vitamin A, and vitamin E) to cyclophosphamide therapy increased the survival of people with small-cell lung cancer treated with cyclophosphamide. It is too early to know if adding antioxidants to cyclophosphamide for cancer treatment is better than cyclophosphamide alone. Vitamin A can be toxic in high amounts. Intravenous injections of the antioxidant, glutathione, may protect the bladder from damage caused by cyclophosphamide. Preliminary evidence suggests, but cannot confirm, a protective action of glutathione in the bladders of people on cyclophosphamide therapy. There is no evidence that glutathione taken by mouth has the same benefits.
As reported here, when laboratory animal and clinical evaluation is the basis for the information, the potential benefits of antioxidants appear. One could say that there has been some backlash at the anti-antioxidant stance promoted by those who quote Dr. Golde and extend his vitamin C research to imply that all antioxidants are problematic for cancer patients. At the Rush Presbyterian St. Luke's Medical Center, the suggestion that vitamin E might inhibit radiation effects was discounted. A press report stated (11):
Vitamin E Does Not Protect Cancer Cells Against Radiation
New York. 15 January 2000 (posted 19 March, 2001). Cancer patients who take vitamin E are probably not hindering the desired effects of radiation, according to a laboratory study done by radiation oncologists at Rush-Presbyterian-St. Luke's Medical Center in Chicago.
Researchers at Rush were concerned that patients who take vitamin E may be inadvertently providing protection for the cancer cells that are the target of radiation therapy. Radiation damage is one form of oxidation, and vitamin E's antioxidant properties presumably extend to cancer cells.
To determine if this were true, Rush researchers, led by Dr. Ed Blazek, director of radiation biology in the Rush department of radiation oncology, grew cells originating from human breast and prostate tumors in nutrient solutions containing several concentrations of vitamin E. The cells were then irradiated with the same daily doses used for patients.
The Rush team found that the tested concentrations of vitamin E did not interfere with the desired killing of cancer cells by radiation. An important limitation of this study, however, is that the level of vitamin E taken up by the cancer cells in laboratory culture has not yet been measured, and might be smaller than the level taken up by cells of a tumor in the patient's body. If so, it is still possible that vitamin E might worsen treatment outcomes.
Although no undesirable protection of cancer cells was found, the researchers issued a caution to those taking vitamin E and other alternative therapies. "Any drug that is taken during cancer radiotherapy or chemotherapy should be tested to prove that it does not protect the tumor cells, defeating the intended effect of the treatment," Blazek said.
Natural extensions of this work would include the addition of the drug pentoxifylline to vitamin E, since this combination has been reported to partially reverse radiation damage to normal tissue, the testing of vitamin C for radioprotection, and the testing of both vitamins E and C for protection from representative cancer chemotherapy drugs.
This research, performed by Drs. Alex Perez and Katherine Baker together with Dr. Blazek, was presented at the annual meeting of the Radiological Society of North America in Chicago.
Then, in a follow-up report from the same hospital, this time including vitamin C (12, 13):
Vitamins C and E Fight Side Effects of Pelvic Radiation for Cancer
March 20, 2001. A small study of 20 men and women suffering from chronic radiation proctitis has shown that daily vitamins E and C substantially reduced or eliminated their symptoms. Proctitis has traditionally been treated with anti-inflammatory agents, without satisfactory results.
Radiation therapy is one treatment option for men with localized prostate cancer and for women with cervix and endometrial cancers. Radiation therapy is effective in killing cancer cells. But the therapy damages also any normal, non-cancerous cells within range of the beam.
Complications are especially common in patients who are treated with older equipment. New, 3D conformal, Intensity Modulated or Proton beam equipment (available in the USA and some other countries) targets the beam much more precisely. Higher doses can be given to tumor with less damage to bladder and rectum.
Most patients take vitamins-does this interfere with killing cancer cells?
Even under the best conditions patients want to do everything possible to protect themselves from radiotherapy side effects. Many patients who undergo cancer treatments take vitamins and supplements. Until recently, oncologists seldom asked patients about this.
Doctors still have almost no evidence on which to advice cancer patients about common supplements. But a previous, laboratory study by radiation oncologists at Rush-Presbyterian-St. Luke's Medical Center found that "Cancer patients who take vitamin E are probably not hindering the desired effects of radiation."
Dr. Keith Bruninga, gastroenterologist at Rush-Presbyterian-St. Luke's has now looked to see how much protection vitamins E and C actually offer patients irradiated for prostate, cervical or endometrial cancer. The effect of the vitamins in the treatment of chronic radiation proctitis had not been studied before, Dr. Bruninga said.
In normal bowel and rectal tissues exposed to radiation for cancer in the pelvis, oxygen radicals form and patients experience the symptoms of proctitis, he said. The condition starts with swollen, inflamed tissue, and it increases with dose. The symptoms, which may include diarrhea, pain, bleeding and incontinence, usually clear up within a few weeks of the last radiation treatment.
However, the symptoms do not clear up in 10-20 percent of patients. Some patients develop symptoms months or years after the initial radiation exposure.
"Our study showed that we can harness the potent antioxidant properties of the vitamins to repair cell damage and bring relief to many people who suffer from the persistent, lifestyle-altering symptoms of chronic radiation proctitis," Dr. Bruninga says in a paper published in the April issue of The American Journal of Gastroenterology.
Oxygen free radicals form from cells that have been injured. Oxygen free radicals are highly active molecules that react with cells by changing or damaging their structure. The formation of the oxygen free radicals increases the amount of injury to the cells and results in a chronic condition as blood flow to the cells is decreased.
Vitamin E is a potent antioxidant that can react with damaging oxygen free radicals. Vitamin C in combination with E increases the effects of vitamin E. The researchers believe that the antioxidant treatment regimen using the vitamins counteracts and can prevent oxygen free radical injury and increase blood flow to the injured cells of patients with chronic radiation proctitis.
Patients in the study, ten men and ten women with chronic radiation proctitis, took one 400 IU vitamin E tablet along with one 500 mg vitamin C tablet three times each day for eight consecutive weeks. Patients purchased the vitamins themselves at the store of their choice.
Each patient in the study rated their symptoms in terms of severity and frequency before and after treatment with the vitamins using a questionnaire developed by the researchers.
The impact of the symptoms on the lifestyle of the patients was also assessed using a questionnaire. Ten of the patients were assessed again after one year to determine if their initial responses were sustained.
The assessments showed a significant improvement in bleeding, diarrhea and urgency after taking the vitamins. Patients with rectal pain did not improve significantly. Thirteen patients reported an improvement in their lifestyle including seven whom reported a complete return to normal.
All of the ten patients who were assessed after one year reported a sustained improvement in their symptoms while continuing to take the vitamins.
The Rush physicians believe that the actual incidence of the ailment is greater than the estimated 10-20 percent of radiation patients. They feel that many patients, relieved and grateful that their cancers are remission, are embarrassed to tell their physicians about the symptoms of radiation proctitis.
Currently, the Rush physicians are seeking additional individuals with chronic radiation proctitis to conduct a larger, double-blinded study of the effectiveness of antioxidants in the treatment of the illness.
"If our continued research shows that the antioxidant regimen is successful in treatment of this illness, we plan to investigate its use to prevent chronic radiation proctitis," said Dr. Bruninga.
Results of the study appear in April 2002 issue of The American Journal of Gastroenterology.
THE ALTERNATIVE: AVOIDING EVEN NORMAL LEVELS OF ANTIOXIDANT INTAKE
One of the early complaints about vitamins and chemotherapy was this one, described just four months before Dr. Golde made his comments at an American Cancer Society Meeting, summarized by a report on prostate cancer (13):
Vitamins and Chemotherapy
Although the antioxidant vitamins A, C, and E help repair damaged cells, it is probably not a good idea to take large amounts during radiation treatment. One object of chemotherapy is to damage cancer cells. Antioxidants, however, appear to counteract the process, according to Dr. Rudolph Salganik's report to the annual meeting of the American Society for Cell Biology (December 1999). He pointed out that "Almost all anticancer drugs kill cancer cells by way of apoptosis, and antioxidants like vitamin A and vitamin E dramatically reduce apoptosis in cancer cells." Patients should therefore avoid taking any more than a normal amount of these vitamins during chemotherapy treatment.
This sounds like reasonable advice-just don't add to normal intake-but Dr. Salganik's own suggestion went further: indicating that an antioxidant-depleted diet could improve cancer therapies. The study referred to above was reported on as follows (14):
Study: avoiding vitamins A, E might improve cancer therapy
By David Williamson, UNC-CH News Services
CHAPEL HILL-Vitamins A and E, which normally boost human health in numerous ways, also appear to keep cancer cells from dying through the natural protective process scientists call apoptosis, new University of North Carolina at Chapel Hill research shows.
As a result, giving patients those vitamins may prevent cancer cells from self-destructing and work against cancer therapy, scientists say.
Researchers at UNC-CH's schools of public health and medicine presented their findings Monday (Dec. 13) during a news conference at the American Society for Cell Biology's annual meeting in Washington, D.C. Drs. Rudolph Salganik, research professor of nutrition, and Terry Van Dyke, professor of biochemistry and biophysics, directed the studies.
"We believe this work is important because it may make cancer treatments more effective," Salganik said. "It suggests that cancer patients, especially those undergoing chemotherapy or radiation therapy, may do better on an antioxidant-depleted diet."
The scientist and his colleagues study reactive oxygen species (ROS), which play a central role in the series of signals that allow cells to kill bacteria and viruses, destroy toxins and trigger the apoptotic "suicide" of defective cells such as cancer, he said. Antioxidants, such as vitamins A and E, protect normal cells from the damaging effects of ROS but apparently also can prevent the targeted apoptotic death of cancer cells that threaten humans and other mammals, the new work suggests.
Other researchers involved were Drs. Craig D. Albright, research assistant professor of nutrition; and Steven H. Zeisel, professor of nutrition and pediatrics and chair of nutrition.
The UNC-CH experiments involved putting mice that were predisposed to developing brain tumors on specially modified diets that were either supplemented with standard amounts of antioxidants or were antioxidant deficient for four months. Researchers then carefully monitored the rodents' health and their brain tumors, if any, to see how the animals fared on the different diets.
Mice receiving extra vitamins A and E showed no benefit in either the size or incidence of brain tumors, Salganik said. They also had relatively short lives.
"Interestingly and more importantly, in animals that received antioxidant-depleted diets, brain tumors were significantly reduced in size because of induction of oxidant stress due to what are commonly called free radicals in the brain tumors," Albright said. "Higher levels of cell death was restricted only to the brain tumors, while normal tissues were not affected by depletion of antioxidants in the mouse diets."
In mice getting low levels of vitamins A and E, no negative effects were seen in normal cells, but about 19 percent of tumor cells showed evidence of apoptosis. In those ingesting normal quantities of antioxidant vitamins, only about 3 percent of tumor cells were apoptotic.
The group's findings may explain two previous clinical studies showing that heavy smokers who ate a diet high in beta-carotene antioxidants had significantly higher rates of lung cancer, Salganik said.
"These new studies raise important issues regarding the advisability of ingesting high levels of antioxidants as a potential anti-cancer benefit," Albright said. "Clearly, more studies are needed at the clinical level in human populations to address the real value of antioxidant supplements or antioxidant depletion in people at risk of developing cancer."
Salganik said he hoped clinical studies would begin within a year or two. Van Dyke is a member of the UNC Lineberger Comprehensive Cancer Center.
Up to this point, no clinical study results along these lines have been reported. The suggestion of starving antioxidants, however, runs contrary to most of the information currently available. The study referred to above, involving heavy smokers and beta-carotene intake has already been the subject of considerable controversy and it appears there were unique factors in this population of heavy smokers in Finland that were studied. Findings to the contrary are common. For example, in a recent evaluation of the risks of lung cancer in relation to various carotenoids ingested. The conclusion was (15):
Lower risks of lung cancer were observed for the highest versus the lowest quintiles of lycopene (28%), lutein/zeaxanthin (17%), beta-cryptoxanthin (15%), total carotenoids (16%), serum beta-carotene (19%), and serum retinol (27%). These findings suggest that high fruit and vegetable consumption, particularly a diet rich in carotenoids, tomatoes, and tomato-based products, may reduce the risk of lung cancer.
SHOULD HERBS BE WORRISOME ADJUNCTS TO CANCER THERAPIES?
There is only one herb that has been implicated in a potential adverse effect on chemotherapy, and its effect has nothing to do with antioxidant activity of the herb. This one herb has been implicated in lowering the dose of a wide range of drugs because it strongly activates the drug-metabolizing enzyme cytochrome P450 CYP3A4. This is St. John's wort (16), which was commonly used for treating depression during the 1990s, but has since become little used due to the concerns for drug interactions (as well as some question about its efficacy). No other herb has been identified as a potential inhibitor of chemotherapy drugs. Although many herbs have some antioxidant potential, their influence over oxidative reactions is low due to the low dosage commonly employed. Unlike vitamin C, which is presented as a pure or nearly pure compound in dietary supplements, herbs contain little vitamin C (in relation to Dr. Golde's concern) and low levels of antioxidant substances. Further they contain little, if any, of the substances that appeared to inhibit cisplatin cytotoxicity in cultured glioma cells. There are no pharmacology or clinical studies showing problems with herbs other than St. John's wort in relation to chemotherapy or radiation therapy. By contrast, the widespread use of herbs and herb extracts to minimize cancer therapy side effects in the Orient is accompanied by extensive favorable reports.
REASONABLE PHYSICIAN'S ADVICE
Cautions that can reasonably be forwarded by physicians are these:
- The use of herbs and dietary supplements, including vitamins and antioxidants, as adjuncts to modern cancer therapies, is an area of ongoing research and, at this time, little is known about the clinical effects.
- Concerns have been raised about use of antioxidants, mainly high doses of vitamin C and high doses of glutathione, based on laboratory experiments suggesting that these substances might impair the full effect of cancer therapies. Clinical studies have not yet revealed any adverse effects, but the concern persists on a theoretical basis, backed up by the laboratory reports; there are also laboratory and clinical reports that suggest that vitamin C and glutathione have positive effects in relation to cancer therapies.
- There is a wide range of recommendations for patient actions based on interpretations of the data available so far. These range from recommendations to administer herbs, vitamins, and other supplements to reduce the adverse effects of cancer therapies without impairing the benefits of the cancer therapies, to maintaining normal healthy dietary recommendations without adding anything, to specifically avoiding antioxidant substances, including those that are normally present in a healthy diet.
- Most medical experts agree that one should not pursue high doses of nutritional supplements or herbs because not enough is known about their potential impact on cancer therapies; their purported benefits may not be confirmed, while there could be risks. However, the only substances for which a strong caution has been repeated are St. John's wort, which may lower the dose of chemotherapy drugs in the body (no impact on radiation therapy is expected), high doses of vitamin C, which might have some protective effect for cancer cells during the therapy, and the antioxidant glutathione, which if taken continuously in large dose might aid cancer cell drug resistance.
In making these comments, physicians should recognize that a wide range of therapies are offered to patients and that the meaning of "high dose" or "continuous use" may vary. For example, physicians should recognize that some proponents of high dose vitamin C therapy recommend huge doses of the vitamin specifically for purported anti-cancer effects. The amounts involved are difficult to consume in one day (e.g., orally consumed up to bowel tolerance, which is typically in the range of 6-12 grams per day). Indeed, some have recommended a continuous vitamin C intravenous drip (8 hours a day) to try inhibiting cancers that are resistant to standard medical therapies (this is after chemotherapy has been suspended). Such huge doses of vitamin C are unproven for effectiveness and could conceivably reduce the impact of concurrent cancer therapies by a number of mechanisms because very high blood levels are attained.
However, most nutritional supplements that involve high doses of vitamin C provide less than 2 grams of the vitamin each day, usually spread over 2 to 3 doses. Blood levels do not rise very much by oral administration, as the vitamin is absorbed gradually and excreted within hours (see Figure 3). There is no evidence that these amounts of oral vitamin C would be harmful for cancer patients. Most proponents of nutritional supplementation, relying upon extensive reports on vitamin C, currently recommend doses of 500-1,500 mg/day. Patients could be cautioned to limit their intake of this particular vitamin to no more than that range.
It is important to note that if cancer cells have a mechanism for absorbing large amounts of vitamin C, and if this is helpful to the growth of cancer cells or to protect against anti-cancer therapies, the amount of vitamin C available in the body normally (baseline of about 60 micromoles/liter) should be sufficient to satisfy the cancer's appetite for it.
Aside from the projected problems with high-dose vitamin C (Dr. Golde did not show inhibition of cancer therapies, only high uptake of vitamin C by cancer cells), there simply is no evidence that other antioxidants (except possibly glutathione), nutritional supplements, or herbs (except St John's wort) inhibit cancer therapies or worsen overall outcomes. To the contrary, they appear to improve outcomes. In the case of St. John's wort, this herb was not proposed as either a treatment for cancer nor a treatment for cancer therapy side effects; rather, it has been used incidentally in the treatment of depression. Thus, no herbs intentionally used as adjuncts to cancer therapy have been implicated in adverse effects clinically.
Even in the case of glutathione, there is reason to believe this substance is not problematic in clinical practice. A concern was raised earlier about supplementation with glutamine, an amino acid that is used to produce glutathione in the body and which is considered a "glutathione-sparing" agent: as glutamine levels increase, glutathione levels are maintained at high levels. Several studies have indicated that glutamine might be a valuable aid to cancer patients, recommended to prevent neuropathy from high dose chemotherapy, to protect the heart from damage due to doxorubicin therapy, and to protect the bowel from damage due to radiation or chemotherapy, but the concern was raised that it would also benefit cancer cells. The studies conducted to date do not support a negative effect for glutamine in relation to cancer. To the contrary, glutamine appears to improve the retention of the chemotherapy drug methotrexate by tumor cells. In one report on this subject, it was concluded that: "These data suggest that oral glutamine supplementation will enhance the selectivity of antitumor drugs by protecting normal tissues from and possibly sensitizing tumor cells to chemotherapy treatment-related injury." The mechanism of action was proposed to be the increase in cellular glutathione related to elevated glutamine levels (18). Dr. VS Klimberg, of the Department of Pharmacology, University of Arkansas, has been a leading researcher in the use of glutamine as a protective agent for cancer patients and has reported widely on its effects. Glutamine and glutathione are currently recommended by many who advocate the use of adjunctive cancer therapies.
Physicians who wish to approach the issue with the most conservative viewpoint could caution patients about extreme therapies, with multiple high dose antioxidants, but cannot with any clinical evidence argue against moderate use of herbs, vitamins, or antioxidants. In fact, the evidence, limited as it may be, is that moderate use of antioxidants is a reasonable approach for patients who are concerned about chemotherapy side effects.
In a recent review of the subject, Kedar Presad and colleagues at the Center for Vitamin and Cancer Research, Department of Radiology, Health Sciences Center, University of Colorado, described the differing views and, as a summary, they pointed out (19):
Radiation therapy is one of the major treatment modalities in the management of human cancer. While impressive progress like more accurate dosimetry and more precise methods of radiation targeting to tumor tissue has been made, the value of radiation therapy in tumor control may have reached a plateau. At present, two opposing hypotheses regarding the use of antioxidants during radiation therapy have been proposed. One hypothesis states that supplementation with high doses of multiple micronutrients including high dose dietary antioxidants (vitamins C and E, and carotenoids) may improve the efficacy of radiation therapy by increasing tumor response and decreasing some of its toxicity on normal cells. The other hypothesis suggests that antioxidants (dietary or endogenously made) should not be used during radiation therapy, because they would protect cancer cells against radiation damage. Each of these hypotheses is based on different conceptual frameworks that are derived from results obtained from specific experimental designs, and thus, each may be correct within its parameters. The question arises whether any of these concepts and experimental designs can be used during radiation therapy to improve the management of human cancer by this modality.
Based on the review of literature, the authors concluded that vitamin C, vitamin E, carotene, and other antioxidants could be useful as a safe adjunct to radiation therapy. Matt Brignall, of the Seattle Cancer Treatment and Wellness Center, where adjunctive therapies are emphasized, also pointed to the evidence supporting the benefit of antioxidants during cancer therapy, saying (20):
Critics of the concurrent use of antioxidants and chemotherapy often point to the lack of clinical trials in humans. Previous preliminary clinical trials, however, have concluded that the antioxidants ginkgo (Ginkgo biloba), melatonin, coenzyme Q10, and N-acetylcysteine did not appreciably reduce the effect of cancer therapies. Pharmaceutical antioxidants, such as amifostine and mesna, have also been extensively studied in conjunction with chemotherapy and radiation, and have not appeared to cause a negative interaction. Many prominent cancer scientists believe that the dietary and pharmaceutical antioxidants prevent some of the worst side effects of cancer treatments.
Further, a common antioxidant now recommended to cancer patients is green tea, which contains an amino acid (theanine) that appears to help retain doxorubicin and other chemotherapy drugs within cancer cells (21). Thus, while it can be reasonable for physicians to offer some limited cautions about use of herbs, vitamins, and antioxidants, they must also be careful not to warn people away from potentially usefully adjunct therapies.
December 2002
REFERENCES
- Leslie M, Vitamin C: How much do you really need?, WebMDHealth, June 19, 2000.
- Cancer tumors shown to consume large amounts of vitamin C. Researchers are cautious about cancer patients taking vitamin C supplements. Memorial Sloan-Kettering Cancer Center, 1999. http://www.mskcc.org/mskcc/html/1166.cfm.
- Russo J, Potential interaction between antioxidants and cancer treatment, http://www.medcomres.com/articles/antioxidants_cancer.htm.
- Roller A, Weller M, Antioxidants specifically inhibit cisplatin cytotoxicity of human malignant glioma cells, Anticancer Research 1998; 18(6A): 4493-4497.
- Cascinu S, et al., Neuroprotective effect of reduced glutathione on oxaliplatin-based chemotherapy in advanced colorectal cancer: a randomized, double-blind placebo-controlled trial, Journal of Clinical Oncology 2002; 20(16): 3478-3483.
- Health Notes, 2000 Healthnotes, Inc.: http://www.hollandandbarrett.com/Drug/Cyclophosphamide.htm.
- Ghosh J, Das S, Role of vitamin A in prevention and treatment of sarcoma 180 in mice, Chemotherapy 1987; 33: 211-8.
- Taper HS, de Gerlache J, Lans M, Roberfroid M, Non-toxic potentiation of cancer chemotherapy by combined C and K3 vitamin pre-treatment, International Journal of Cancer 1987; 40: 575-9.
- Jaakkola K, Lahteenmaki P, Laakso J, et al., Treatment with antioxidant and other nutrients in combination with chemotherapy and irradiation in patients with small-cell lung cancer, Anticancer Research 1992; 12: 599-606.
- Nobile MT, Vidili MG, Benasso M, et al., A preliminary clinical study of cyclophosphamide with reduced glutathione as uroprotector, Tumori 1989; 75: 257-8.
- Rush Presbyterian St. Luke's Medical Center, Vitamin E does not protect cancer cells against radiation, January 15, 2000, PSA Rising Magazine, http://psa-rising.com/medicalpike/ebr/andvitEC031901.shtml.
- Rush Presbyterian St. Luke's Medical Center, Vitamins C and E does fight side effects of pelvic radiation for cancer, March 20, 2001, PSA Rising Magazine http://psa-rising.com/medicalpike/ebr/vitE-C-proctitis031901.shtml.
- Dykes B, Hypertext Guide to Prostate Cancer, Chemotherapy: vitamins and chemotherapy, 2001, http://www.hypertext.org/ENGLISH/ADVANCED.html.
- Williamson D, Study: Avoiding vitamins A, E might improve cancer therapy, University of North Carolina News Services, December 13, 1999, http://www.unc.edu/news/newsserv/research/dec99/salganik121399.htm.
- Holick CN, et al., Dietary carotenoids, serum beta-carotene, and retinol and risk of lung cancer in the alpha-tocopherol, beta-carotene cohort study, American Journal of Epidemiology 2002; 156(6): 536-547.
- Mathijssen RH, Effects of St. John's wort on irinotecan metabolism, Journal of the National Cancer Institute 2002; 94(16): 1187-1188.
- Levine M, et al., Criteria and recommendations for vitamin C intake, Journal of the American Medical Association 1999; 281:1415-1423.
- Rouse K, Glutamine enhances selectivity of chemotherapy through changes in glutathione metabolism, Annals of Surgery 1995; 221(4): 420-426.
- Prasad KN, et al., Pros and cons of antioxidant use during radiation therapy, Cancer Treatment Reviews 2002 28(2): 79-91.
- Brignall M, Is it safe to use antioxidant supplements with chemotherapy?, Healthnotes Newswire, October 10, 2002.
- Sadzuka Y, et al., Enhancement of the activity of doxorubicin by inhibition of glutamate transporter, Toxicology Letters 2001; 123(2-3): 159-67.
APPENDIX 1. BASIC UNDERSTANDING OF THE CANCER THERAPIES
The precise mechanisms of cancer therapies are not fully worked out, though considerable information is available. The following is an overview, based on the author's understanding, indicating the potential role of herbs, vitamins, and antioxidants in preventing side effects of cancer therapies without impairing anticancer treatment.
Radiation
Standard external radiation therapy pinpoints a beam of intensely energetic photons (x-rays, gamma-rays or beta-rays) to a tumor site (see Figure 4). The radiation dose at the focal point is lethal to the cells. Some of the radiation directly breaks up cellular DNA and other components in the target area; it is estimated that about one-third of the damage is direct destruction of critical molecules, leading to inability of the cell to reproduce or to prompt cell death. The primary damage to the tumor, however, comes from generation of a huge number of free radicals that interact with cellular components and disrupt them. These free radicals are mostly generated from water, because it is the most abundant substance in the cells. Because of the beam intensity at the focal point, no amount of antioxidant activity from orally ingested supplements is likely to be able to save these cells.
External radiation therapy is usually administered over an extended period, with several treatments spaced out with many days interval between. The reason that the whole task is not performed with one treatment is that the collateral damage from the radiation would be so severe as to threaten the patient's survival. As it is, when the beam enters the body on its way to the tumor site and exits beyond the tumor, and spreads a bit on either side of the target, the collateral damage is notable and can be extreme. The skin becomes burned and delicate internal organs can become severely damaged and almost unusable. For example, radiation to the throat area can make swallowing virtually impossible; abdominal radiation can cause intestinal ulceration that doesn't heal for months if at all. Still, these off-target tissues are able to repair somewhat between the treatments thanks to the more limited damage at these sites compared to at the tumor itself. As the distance from the beam's focal point increases, there is greater chance to protect the cells with antioxidants that are able to handle the small number of free radicals that are generated.
There are other types of radiation therapy, including brachytherapy, in which radioactive material is inserted into the tumor (as commonly employed for prostate cancer): the radiation spreads out around radioactive "seeds" and kills all cells in the surrounding area, with reduced damage the greater the distance from the radiation source. There are now proton and neutron beams that have a higher proportion of damage caused by direct strikes at DNA and other cellular components, with less reliance on free radical generation.
It is a desired outcome that the collateral damage from all radiation techniques be minimized, which is a potential valuable role for antioxidants. The chances of antioxidants protecting the tumor cells are minimal; there is simply too much radiation at the target. Failures of radiation therapy are mostly attributable to metastasis of the cancer cells (before radiation begins) rather than failure of the radiation to destroy every cancer cell at the target tumor site. No amount of antioxidant therapy nor the reverse-complete avoidance of antioxidant therapy during radiotherapy-will have an impact on this metastasis that has occurred before radiation therapy. Metastatic cells can not be detected by current means and may not reveal themselves for months or even years, which is why cancer therapies are not considered a true success until 5 years pass without sign of new tumor growth, usually at a different site.
One cannot know for certain what effect-good or bad-antioxidants will have on the effects of radiation therapy, without extensive clinical testing that may take years. The concept that tumor cells can be protected is largely based on the assumption that antioxidants are extremely efficient. They would have to clean up the reactive oxygen species as fast as they are produced. Yet, the very large amount of antioxidant research conducted over the past decade clearly shows that these substances have limited impact for several diseases. Where they were thought to have the potential to treat diseases, they have not been very successful, and where they are thought to prevent diseases, they appear effective so long as the exposure to the antioxidants is for years and years, having a continuous mild impact. Antioxidants can be expected to provide some aid to cells unintentionally caught in the periphery of radiation therapy, but, even there, complete protection is not expected due to limited effects.
Chemotherapy
As with radiation therapy, chemotherapy is administered over an extended period, often (though not always), with a duration of several days or weeks between treatments. As with radiation therapy, the task cannot be accomplished all at once, because a lethal chemotherapy dose for the entire tumor would also be lethal for the patient. In fact, one of the key measures of the patient's ability to continue chemotherapy is recovery of the white blood cell count that has been impaired by the drug therapy (this does not apply to some of the new immune based and genetic therapies). Chemotherapy is usually not as focused as radiation therapy on the tumor, and affects the entire body (commonly causing hair loss, distress of the gastro-intestinal system, white blood cell depletion, and fatigue). An adjunctive treatment that protects non-target cells (normal cells) might also protect cancer cells. However, as occurs with radiation therapy, there is a difference between the intensity of the drug action on cancer cells and on other cells, such as bone marrow cells. Otherwise, once the cancer was destroyed successfully, the bone marrow would also be destroyed (which is, in fact, one of the radical chemotherapy approaches, but not the first line treatment). Chemotherapy drugs are selected for clinical use on the basis that they have a more potent action on cancer cells than on other cells. Thus, after the cancer is destroyed, hair grows back, digestion returns to normal, and the immune system functions fully once again. Protection that helps the bone marrow does not necessarily have the potency to protect the cancer cells. Failure of chemotherapy is often the result of the presence of some resting cells, usually cells outside the active tumor mass, that do not respond to chemotherapy drugs. The drugs usually interact with replicating DNA and might miss such individual metastatic cells that are quiescent.
Polysaccharides from herbs have been used for protecting the bone marrow in cancer patients undergoing chemotherapy in China, Japan, and other countries for many years. The clinical study reports indicate improved outcomes (better survival) in patients who utilize this adjunct therapy. It can be argued that the study methodology is inadequate to support the improved survival, and it can be argued that the valid outcomes might be clinically insignificant, so that there is little or no interest in pursing this approach here. But, there is no evidence that bone marrow protection leads to negative effects in terms of tumor destruction or survival rates.
A positive role for antioxidants in the case of chemotherapy drugs is protection against a variety of undesired secondary effects, particularly neuropathy and cardiac damage. The chemotherapy drugs do not function as oxidants, but, rather, influence the cellular DNA and RNA (see Figures 5-6). Except in one in vitro study cited above for glioma cells that are normally resistant to chemotherapy, there is no evidence that antioxidants worsen the outcome of cancer chemotherapies. To the contrary, there is some evidence of protection for secondary effects. Dr. Golde's in vitro research on vitamin C did not show that this substance impaired cancer therapies, only that cancer cells seem to "soak up" the vitamin. His results may not translate to an impairment of the effects of radiation therapy or chemotherapy.
The essential factor in both radiation therapy and chemotherapy is the specificity of the treatment for cancer cells. Antioxidants, herbs, and other kinds of natural supplements are being applied to protect cells that are unintentionally damaged by cancer therapy where the damage is substantially less severe than that caused to the cancer cells. The ability to provide protection for non-target cells without interfering with the damage to cancer cells is based largely on the differential. One may expect that where a cancer therapy is equally lethal to target and non-target cells, that a therapy protective of the non-target cells might also be protective of the target cells. Despite the apparent protection offered by antioxidants and herbs to non-target cells, their abilities to provide that protection are limited. Patients still experience side effects; they are only reduced in intensity. The ability of these same substances to protect target cells is far less, which explains why there hasn't been a sudden failure of cancer therapies during the past decade when millions of people have turned to routine use of supplements with vitamin C, vitamin E, and other antioxidants.
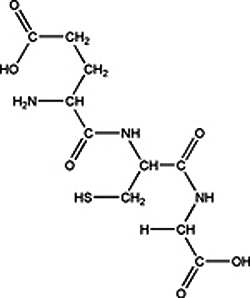
Figure 1. Glutathione

Figure 2. Platin drugs; cisplatin, top; carboplatin, middle; and oxaliplatin, bottom.

Figure 3. Vitamin C bioavailability in plasma after IV administration (black dots)
and oral administration (white dots) with 200 mg (top graph) or 1,250 mg (bottom graph).

Figure 4. Computer modeling of radiation therapy beam
focusing for treatment of a brain tumor.

Figure 5. Mechanism of 5-FU, a common chemotherapy drug. 5-FU is activated by
metabolism to RNA and DNA forms, which then incorporate into the cellular
RNA and DNA, inactivating it or producing toxic rather than normal products.
Figure 6. Oxaliplatin (represented by hexagon units with two prongs)
attaches to DNA strands and blocks their replication,
halting cellular reproduction and leading to cell death.